A 65yr old male with lower back ache
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
Cheif complaints:A 65 yr old male resident of miryalaguda farmer by occupation came with cheif complaints of lower back ache since 4 yrs.
Hopi: patient was apparently asymptomatic 4yrs ago then he developed lower back ache and lower abdominal pain,which is insidious in onset ,continuous,non progressive, partially relieved on medication.
4 yrs back when he developed pain it was associated with fever and burning micturation for which he went to the hospital where ho got diagnosed with htn .he takes antihypertensive drugs whenever he gets dyspnea and weak,blurring of vision and doctors also told he has some kidney problem .
From then he started using painkillers for lower backache partially it relieves. whenever pain exaggrates he takes injection one dose in the hospital (it work for 7 days)he discontinue the tablet for same 7 days and continued till date
7 months back he developed fever and burning micturation for which he went to the hospital where he was diagnosed with CKD and medication were given
Decreased urine output since 7months.
Itching all over the body since 7 months for which he is using medicine ( it relieves partially)
Past history
Diagnosed with CKD 7 months ago andhtn 4 yrs ago
Not a known case of dm,thryoid, epilepsy asthma
No h/o surgeries,no h/o blood transfusion
Daily routine: 4 yrs back he used to go for farming now he stays at home wakes at 6am daily, his diet contains rice, vegetables sometimes meat , evening he drinks tea and he passes all his time with his neighbours and his family and sleeps by 9pm.
Family history: not relevant
Treatment history:atarax-for itching
Oferol,foxstat for increased uric acid level,flodart,sobiup, painkillers
Personal history:
Appetite: decreased
Diet:mixed
Bowel movements-regular
Bladder movements: decreased urine output since 7months
Addictions: he stopped drinking alcohol and smoking from past 15 yrs
General examination
Patient is conscious,coherent,cooperative
Pallor-present
Icterus-absent
Clubbing -absent
Lymphedenopathy-absent
Generalized edema-absent
Vitals: bp-160/80 mmHg
HR:60beats/min
RR:16cycles/min
Temperature: afebrile
Spo2:100 at room temperature
GRBS:110mg%
Systemic examination :
Abdominal examination
On Inspection
Shape of abdomen :-scaphoid
Umbilicus is inverted.
No scars , engorged veins.
All parts of abdomen are moving equally with respiration
On palpation:- all inspectory findings are confirmed.
abdomen is soft, tender in hypogastrium and lower back.
On bimanual examination of kidney- kidney is not palpable.
On percussion:- no shifting dullness and no fluid thrills.
On auscultation:- normal bowel sounds are heard.
Respiratory examination:
Trachea-central
Bilateral air entry present
Vesicular breath sounds are heard
No added sounds
Cvs:
Apical impulse present
S1,s2 are heard
CNS:HIGHER MENTAL FUNCTIONS-
Normal
Memory intact
CRANIAL NERVES :Normal
SENSORY EXAMINATION
Normal sensations felt in all dermatomes
MOTOR EXAMINATION
Normal tone in upper and lower limb
Normal power in upper and lower limb
Normal gait
REFLEXES
Normal, brisk reflexes elicited- biceps, triceps, knee and ankle reflexes elicited
CEREBELLAR FUNCTION
Normal function
No meningeal signs were elicited
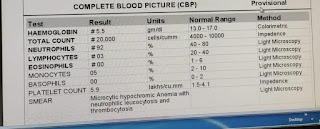
Previous hospital investigations :
Diagnosis:ckd secondary to nsaids,htn









Comments
Post a Comment