A 55yr old male with sob
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome.”
Case:A 55 yr old male toddy tree climber by occupation came to OPD with cheif complaints of
sob at rest since 2 days
High grade fever since 2 days
Dry cough since 1day
HopI:
Patient was apparently asymptomatic
3yrs ago then he developed sob( grade -1)mmrc which is insidious in onset,non progressive till 10/4/23
Aggrevated on exposure to cold weather and dust relieved on medication and on rest
Not associated with orthopnea and pnd
On 10/4/23 patient developed sob( grade -4) which is sudden in onset ,non progressive associated with wheeze
No aggrevating and relieving factor
H/o High grade fever since 2days sudden in onset, intermittent,not associated with chills and rigors and relieved on medication
H/o dry cough since 1day
No H/o chest pain, haemoptysis
No significant family history
Shape of the chest -round
Trachea appears to be central
Usage of accessory muscles -present
No dropping of shoulders
No crowding of ribs.
Apex impulse is not observed
Palpation
No local rise of temperature
No tenderness
Trachea -central
Chest movements -equal on both sides
Ap diameter-28cm
Transverse diameter -32cm
Chest circumference:
Inspiration:87cm
Expiration :85cm
Chest expansion:2cm
Percussion:
Rt. Lt
SCA. Resonant. Resonant
ICA. R. R
MA. R. Dull
IMA. Dull. Dull
AA. R. R
IAA. R. R
SSA. R. R
ISA. R. R
Infra SA. R. R
Auscultation : bilateral rhonchi are heard in MA,IAA,ISA,inter SA
CVS:
S1,S2 are heard
No murmurs
Per Abdomen:
Shape is scaphoid
Abdomen is soft and non tender with no signs of organomegaly
Bowel sounds are heard
CNS:
HIGHER MENTAL FUNCTIONS-
Normal
Memory intact
CRANIAL NERVES :Normal
SENSORY EXAMINATION
Normal sensations felt in all dermatomes
MOTOR EXAMINATION
Normal tone in upper and lower limb
Normal power in upper and lower limb
Normal gait
REFLEXES
Normal, brisk reflexes elicited- biceps, triceps, knee and ankle reflexes elicited
CEREBELLAR FUNCTION
Normal function
No meningeal signs were elicited
Investigations:LFT
TB:0.54mg/dl
DB:0.2mg/dl
ALT:247IU/l
ALP:176IU/l
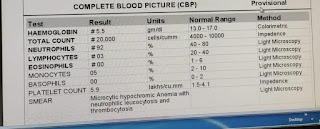
Hb:12.6gm/dl
TLC:11,000
Plt count:2.4lakhs
Provisional diagnosis:excerbation of copd, type 1 respiratory failure
Rx
O2inhalation with face mask 4-6lit/min to maintain spo2-95
Syp.grillincitus tid
Inj.piptaz 4-5gm IV tid
Pantop 40mg- bbf
T.shelcal od
Lidiliv 300mg bd
Inj hydrocort 100mg 2hrs after meal




Comments
Post a Comment